.full-width
goal
TREATMENT GOALS OF ATOPIC DERMATITIS (ECZEMA)
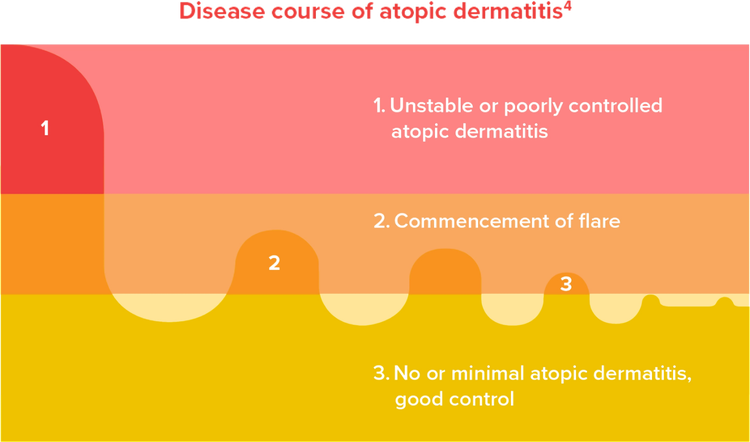
Since atopic dermatitis is a chronic disease with relapses and no cure currently, it is important to set treatment goals with your doctor to control and relieve symptoms of your atopic dermatitis in the long term.1,3,4
The key treatment goals of atopic dermatitis include4:
- Reduction of extent and severity of atopic dermatitis
- Prevention and reduction of relapse – Maintain remission
- Control of signs and symptoms
- Clearance of skin lesions – Return to normal barrier
- Improvement of quality of life – Reduce burden of disease
- Prevention of complications (eg, infection chronicity)
Do keep in mind that it is important to consult your doctor if you have symptoms of atopic dermatitis and if it is affecting your sleep or daily activities.1,3 Your doctor will determine and provide diagnosis based on your symptoms, lifestyle, as well as medical and family history.5,6 Sometimes, your doctor may refer you to a dermatologist for therapies to better manage your atopic dermatitis.2
method
TIPS TO IMPROVE
YOUR ATOPIC DERMATITIS (ECZEMA)
The first step to treating atopic dermatitis is to take care of your skin properly.2,5 Here are some skin care tips that might help.
Avoid scratching the skin2,7
- Keep your nails short or wear gloves might help prevent skin damage from unintentional scratching2,7
Avoid things that might trigger symptoms of your atopic dermatitis2,6,7
- These triggers vary from person to person.8 They could include irritants (eg, soap, detergent and wool), sudden temperature changes, or emotional stress6,7
- Speak to your doctor to identify and avoid your triggers to prevent flare-ups2,9
Prevent irritating your skin when showering/bathing7,10
- Avoid long and hot shower/bath.6,10 Take short, lukewarm shower instead7,10
- Avoid scrubbing your skin too hard7,10
- Use gentle body washes and cleansers, or replacements recommended by your doctor7,10
- Apply emollients (lotions, creams, or ointments) after shower immediately to prevent your skin from drying out6,7
Keep your skin hydrated with emollients (lotions, creams, or ointments)2,5,7
- Emollients help moisturize the skin, heal cracks in the skin, and reduce symptoms like dry skin, itchiness and redness2,9
- Apply emollients twice a day or more if needed.2,6 Avoid products that contain alcohol, scents, dyes, fragrances, and other skin-irritating chemicals7
- Consult your doctor/pharmacist for recommended emollients that are suitable for you.2 You might have to test out a few before finding the most suitable one.2 At times, you may have to switch to another product if it becomes less effective over time2
medication
MEDICATIONS AND THERAPIES FOR ATOPIC DERMATITIS (ECZEMA)
You might also need additional medications or therapies to help control your atopic dermatitis, including topical treatments, oral medications, injectables, and other therapies.5
Each treatment option is associated with its own advantages and limitations, thus warranting careful consideration prior to administration.11 Your doctor will evaluate the severity of your condition and develop a personalized treatment plan for you.11
.en-margin
serious
medication-1.svg/ If your atopic dermatitis is mild to moderate/161/149
If your atopic dermatitis is mild to moderate:
Topical medications might be helpful. They are treatments that can be directly applied to the skin, including topical corticosteroids, topical calcineurin inhibitors and topical PDE4 inhibitors.2,6,12,13 They can help control symptoms and repair your skin.5 Follow your doctor’s instructions and/or those in the patient information leaflet of your medication on when and how to apply them.2
Topical corticosteroids
- They can help reduce inflammation in a few days2
- Various options are available and they come in different strengths.2,6 You may need different corticosteroid prescriptions, depending on the severity of your atopic dermatitis and the areas of skin affected2
- You may experience a mild stinging sensation as you apply them.2 Occasionally, topical corticosteroids may also cause thinning of the skin, changes in skin color, acnes and increased hair growth.2 However, most of these side effects will improve once you stop your treatment2
Topical PDE4 inhibitors
- They are a type of nonsteroidal, anti-inflammatory, topical ointment that contains PDE4 inhibitors (an immunosuppressant), which blocks a chemical that can cause the flaring of atopic dermatitis14–16
- They are suitable for adults and children above 3 months of age13,16
- They can be used over a long period on time13
- They can be used in sensitive skin and more delicate body areas such as face, eyelids, genitals, and skinfolds13,16
- The most common side effect is burning or stinging in the area you apply them and should go away after using the treatment for a while13,14
Topical calcineurin inhibitors
- They are a type of topical ointment that contains calcineurin inhibitors (an immunosuppressant), which blocks a chemical that can cause the flaring of atopic dermatitis12,17
- They may be used when other topical treatments have failed.14,17 They are also useful in sensitive areas such as face and groin, in adults, and in children above 2 years of age6,12
- Avoid strong sunlight when using these ointments5,12,14
- You might experience burning or stinging sensation, redness, or itching in the area you apply them that generally disappear within one week of use.12,14 They might also cause tingling skin, a change in skin color, and cold sores or warts14
Very serious
medication-2.svg/ If your atopic dermatitis is moderate to severe/149/149
If your atopic dermatitis is moderate to severe:
Your doctor would modify and step up your treatment plan by including systemic therapies such as systemic immunosuppressants, phototherapy and biologics.11 Follow your doctor’s instructions on when and how to take them.
Conventional therapies
These therapies include systemic corticosteroids, traditional immunosuppressants and phototherapy.18
Systemic immunosuppressants
In people with atopic dermatitis, their immune systems would overact to certain substances such as dust and pet fur.14 Immunosuppressants work by reducing the activity of your immune system, which help control your atopic dermatitis.14,19
-
Steroids
- They can be used to reduce swelling, relieve itching and help your skin heal14
- Potential serious side effects could occur due to inappropriate use.6,11 If steroids are prescribed, you should follow your doctor’s instruction strictly
-
Traditional systemic medications
- They are oral or injectable medications19
- In most cases, your doctor may stop the treatment and switch you to topical medications once your atopic dermatitis is controlled19
Phototherapy (also known as light therapy or ultraviolet light therapy)
- Phototherapy involves exposing the affected skin to controlled amounts of natural sunlight, artificial ultraviolet A (UVA) or narrow band ultraviolet B (UVB) alone or with drugs5
- It is only recommended in patients with severe atopic dermatitis, such as those who do not get better with other treatments, or whose symptoms reappear quickly after treatment5,6
- Long-term phototherapy can cause harmful effects, including premature skin aging, changes in skin color, and an increased risk of skin cancer5
- To learn more, discuss with your doctor about the risk and benefits of receiving phototherapy5
Targeted therapies
Targeted therapies work by targeting specific components of the inflammatory pathway that cause atopic dermatitis in the body.20 These include biologics and oral Janus kinase inhibitors.21
Biologics
- They are medicines that are produced from living organisms or contain components of living organisms.22 It works by targeting specific chemical messengers in the body that cause symptoms of atopic dermatitis23,24
- They could be an option for adults and children with moderate-to-severe atopic dermatitis who do not respond to other treatments5,6,24
- They can help reduce itch and improve skin condition23
- Common side effects include conjunctivitis, cold sores, and infection at the injection site24
Oral Janus kinase (JAK) inhibitors
- They work by blocking the transmission of immune signals involved in atopic dermatitis19
- They are for people with moderate to severe atopic dermatitis14,19
- Compared with biologics, they provide faster and more effective symptomatic relief (such as itch) and help improve the skin condition25,26
- Across different clinical studies, a significant improvement in quality of life was observed in patients taking JAK inhibitors25,27
- Common side effects include nausea, vomiting, headache, and cold sores14
Wet wrap therapy
Wet wrap therapy can be considered as part of the acute treatment to gain control in some patients with severe AD.11
- It is a method that can quickly reduce the severity of atopic dermatitis18
- Wearing wet dressings can help soothe and hydrate the skin, reduce itching and redness, prevent scratching, and allow the skin to heal2,6
- This therapy involves applying emollients or topical corticosteroids (or both), sealing it with a wet gauze and covering it with a dry garment over the affected skin5,18
- Dressings can be worn for a few days, overnight, or during the day.6 In general, you would need to change to a fresh dressing every 8 hours.6 Follow your doctor’s instruction on the exact frequency and dressing steps5
References
- NHS. Atopic eczema: Overview. Available at: www.nhs.uk/conditions/atopic-eczema/, Accessed Oct 2025.
- NHS. Atopic eczema: Treatment. Available at: www.nhs.uk/conditions/atopic-eczema/treatment/. Accessed Oct 2025.
- Mayo Clinic. Atopic dermatitis (eczema): Symptoms & causes. Available at: www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/symptoms-causes/syc-20353273. Accessed Oct 2025.
- Rubel D, et al. J Dermatol 2013;40:160-171.
- Mayo Clinic. Atopic dermatitis (eczema): Diagnosis & treatment. Available at: www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/diagnosis-treatment/drc-20353279. Accessed Oct 2025.
- UpToDate. Patient education: Eczema (atopic dermatitis) (Beyond the Basics). Available at: www.uptodate.com/contents/eczema-atopic-dermatitis-beyond-the-basics. Accessed Oct 2025.
- National Institute of Allergy and Infectious Diseases. Eczema (atopic dermatitis) treatment. Available at: www.niaid.nih.gov/diseases-conditions/eczema-treatment. Accessed Oct 2025.
- NHS. Atopic eczema: Causes. Available at: www.nhs.uk/conditions/atopic-eczema/causes/. Accessed Oct 2025.
- American Academy of Dermatology Association. Can anything relieve severe atopic dermatitis? Available at: www.aad.org/public/diseases/eczema/insider/severe-atopic-dermatitis. Accessed Oct 2025.
- Student Health Service, Department of Health. Health information: Other health issues (eczema). Available at: www.studenthealth.gov.hk/english/health/health_ophp/health_ophp_tet.html. Accessed Oct 2025.
- Boguniewicz M, et al. Ann Allergy Asthma Immunol 2018;120:10-22.
- National Eczema Society. Topical calcineurin inhibitors (TCIs). Available at: eczema.org/information-and-advice/treatments-for-eczema/topical-calcineurin-inhibitors/. Accessed Oct 2025.
- National Eczema Association. Available at: nationaleczema.org/. Accessed Oct 2025.
- WebMD. Immunomodulators for atopic dermatitis. Available at: www.webmd.com/skin-problems-and-treatments/eczema/immunomodulators-atopic-dermatitis. Accessed Oct 2025.
- Yang H, et al. JAMA Dermatol 2019;155:585-593.
- WebMD. PDE-4 inhibitors for atopic dermatitis. Available at: www.webmd.com/skin-problems-and-treatments/eczema/atopic-dermatitis-pde4-inhibitors. Accessed Nov 2025.
- Drugs.com. Calcineurin inhibitors. Available at: www.drugs.com/drug-class/calcineurin-inhibitors.html. Accessed Nov 2025.
- Calabrese G, et al. Dermatol Pract Concept 2022;12:e2022155.
- National Eczema Association. Prescription oral. Available at: nationaleczema.org/eczema/treatment/immunosuppressants/. Accessed Oct 2025.
- Kalamaha K, et al. Expert Rev Clin Immunol 2019;15:275-288.
- Bieber T. Nat Rev Drug Discov 2022;21:21-40.
- MedicineNet. Biologics (biologic drug class). Available at: www.medicinenet.com/biologics_biologic_drug_class/article.htm. Accessed Nov 2025.
- Deleanu D & Nedelea I. Exp Ther Med 2019;17:1061-1067.
- WebMD. Biologics for atopic dermatitis. Available at: www.webmd.com/skin-problems-and-treatments/eczema/biologics-atopic-dermatitis. Accessed Nov 2025.
- Traidl S, et al. Allergol Select 2021;5:293-304.
- Bieber T, et al. N Engl J Med 2021;384:1101-1112.
- Thyssen JP, et al. J Eur Acad Dermatol Venereol 2022;36:434-443.